Most people spend about 33% of their lives snoozing away. For those with insomnia, though, that percentage can be smaller. In fact, most experts agree that about 30% of adults in the United States struggle with this condition. That makes insomnia perhaps the most common sleeper-related disorder in the country.[1,2]
Despite it being so common, many struggle with understanding their condition and finding effective treatment. From prescription sleeping pills to over-the-counter remedies, many people search for that magical sleep aid to help them finally get some shut-eye. Unfortunately, many people can try and try various methods for inducing sleep without luck. Research suggests, though, that there is an incredibly effective method for treating this condition: CBT-I, or cognitive behavioral therapy for insomnia.
Before examining why CBT-I is so effective, though, it’s first necessary to take a look at both insomnia and CBT in closer detail.
What is Insomnia?

Insomnia is a condition where someone has difficulties falling asleep and/or staying asleep. Insomnia can be either short-term (acute) or long-term (chronic). Now, there are two classifications of insomnia: primary and secondary. Primary insomnia is sleeplessness that is not due to another underlying condition, whereas secondary insomnia is the result of another medical problem. Notably, insomnia is not just objectively poor sleep but also the subjective perception of poor sleep.
If you feel like you’re having trouble sleeping, take our insomnia test.
Symptoms
Insomnia symptoms can include:
- Early wakings
- Less time spent asleep
- Frequent night wakings
- Feeling fatigued upon waking
- Delayed sleep onset latency, or extended time falling asleep
- Daytime sleepiness
- Constant or near-constant fatigue[3]
Why Do People Develop Insomnia?
Why do people have insomnia? Well, it depends based on the individual. For example, acute insomnia may be the result of a stressful life experience; sleep problems may disappear once the period of stress ends.
Chronic primary sufferers, though, typically have three factors in common. Based on the widely accepted Spielman model, there are three P’s that place someone at risk for developing insomnia. These factors include predisposition (such as genetics or specific personality traits), a precipitating trigger (usually whatever caused the acute episode), and perpetuating poor sleep hygiene habits and behaviors first developed in response to the acute episode.[4,5] In other words, some people are just more predisposed to sleeplessness than others. Furthermore, those who suffer from an acute episode may form poor coping strategies to deal with this initial sleeplessness. Then, these strategies become habitual. This in turn reinforces poor sleep habits (sleep hygiene) that make it harder and harder to sleep as time goes on.
So, just who is at the greatest risk for developing insomnia? Those at higher risk include:
- Elderly people
- Women
- African Americans
- Long-distance travelers
- Sedentary individuals
- Lower-income households
- Those who work night shifts or inconsistent shifts[6]
What are the dangers of untreated insomnia?
Sleep is incredibly vital to overall health and wellbeing. When sleep is disrupted long-term, it can lead to some significant health risks, including high blood pressure and diabetes.[7] In some rare cases, people may eventually not be able to sleep at all, which ultimately leads to death. Called fatal familial insomnia, this condition is genetic. Again, though, this specific form of sleeplessness is incredibly rare.[8]
However, someone’s physical health isn’t all that suffers from sleep deprivation; mental health can decline, too. Those with insomnia, for instance, are at increased risk for developing conditions like depression. In fact, those who recover from all symptoms of depression except for insomnia are much more likely to relapse than those who can sleep well. If someone’s condition persists, insomnia can also greatly increase suicide risk.[9,10]
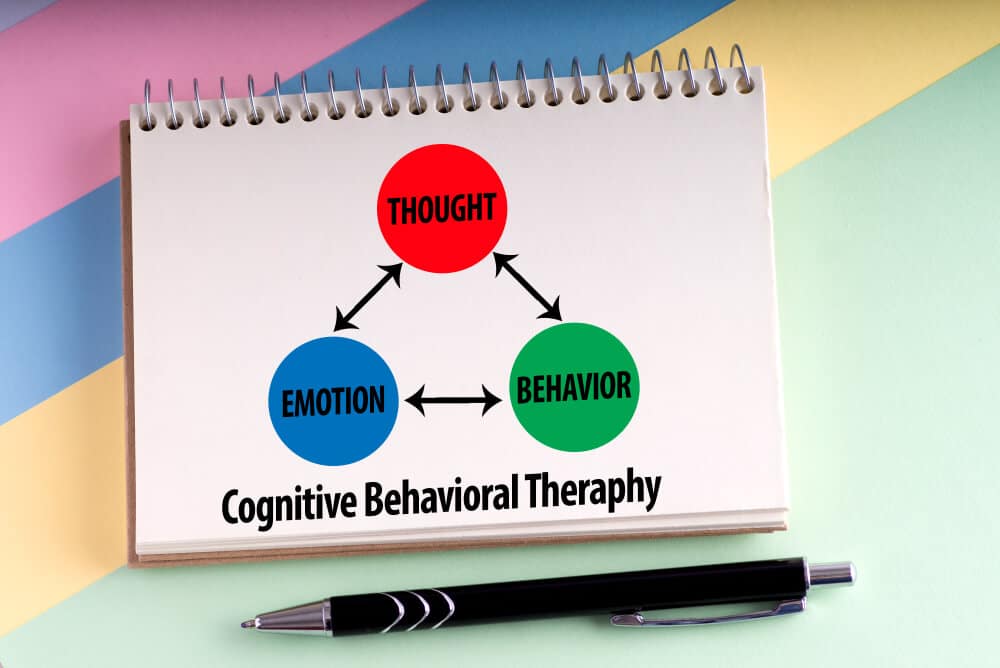
What is CBT?
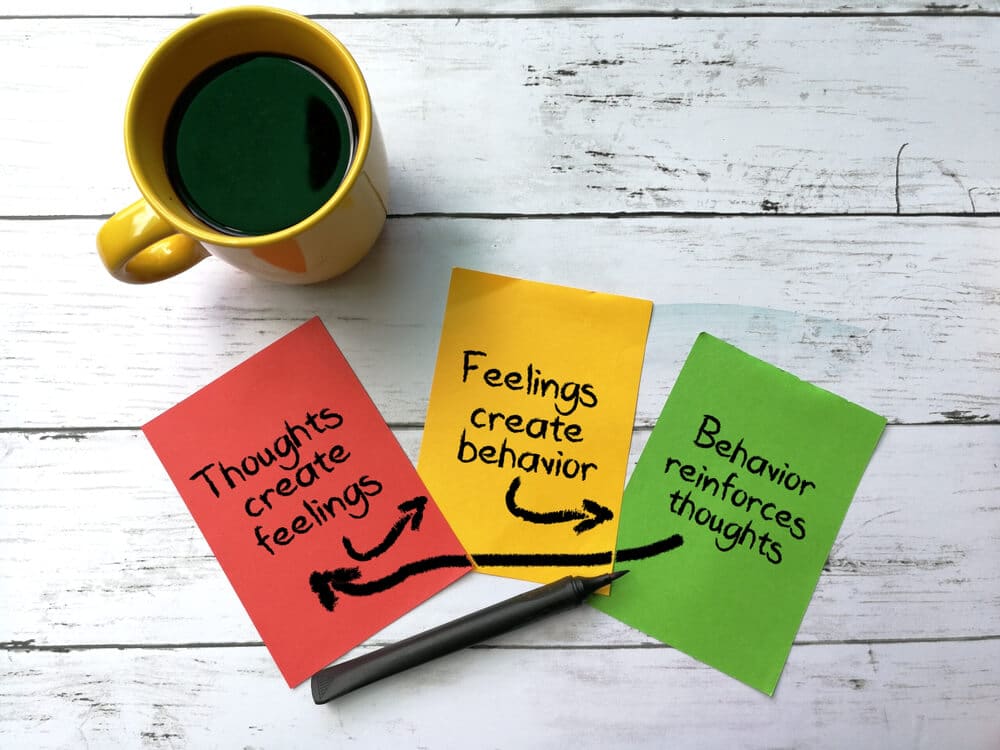
CBT stands for cognitive behavioral therapy. It is a form of talk therapy that involves a patient recognizing thought patterns, habits, and behaviors, then challenging them. This challenge involves changing unwanted or unhelpful behaviors, which can mean learning coping strategies as well as learning how to better manage emotions. So, CBT rests on the idea that thoughts, behavior, and feelings are all closely related. That means better managing all three can result in an improved sense of wellbeing.[11]
What is CBT-I?
CBT-I stands for cognitive behavioral therapy for insomnia. It follows the same basic principles as standard CBT; namely, that thoughts, feelings, and behavior all intertwine. However, it focuses specifically on aspects of life that affect sleep. In other words, CBT-I forces patients to reconsider their thought patterns, emotions, and habits in relation to sleep. The goal, of course, is to improve rest time and/or quality.
How Effective is CBT-I?
CBT-I is incredibly effective for treating insomnia.[12,13] In fact, one study showed that a majority of its participants experienced both subjective and objective improvements in rest. This research even suggests that CBT-I-developed skills may help someone improve other issues, such as anxiety.[14] This effectiveness is why the American Academy of Sleep Medicine (AASM) recommends CBT-I as the first line of treatment for this condition—ahead of even prescription medications.[15]
How Does CBT-I Work?
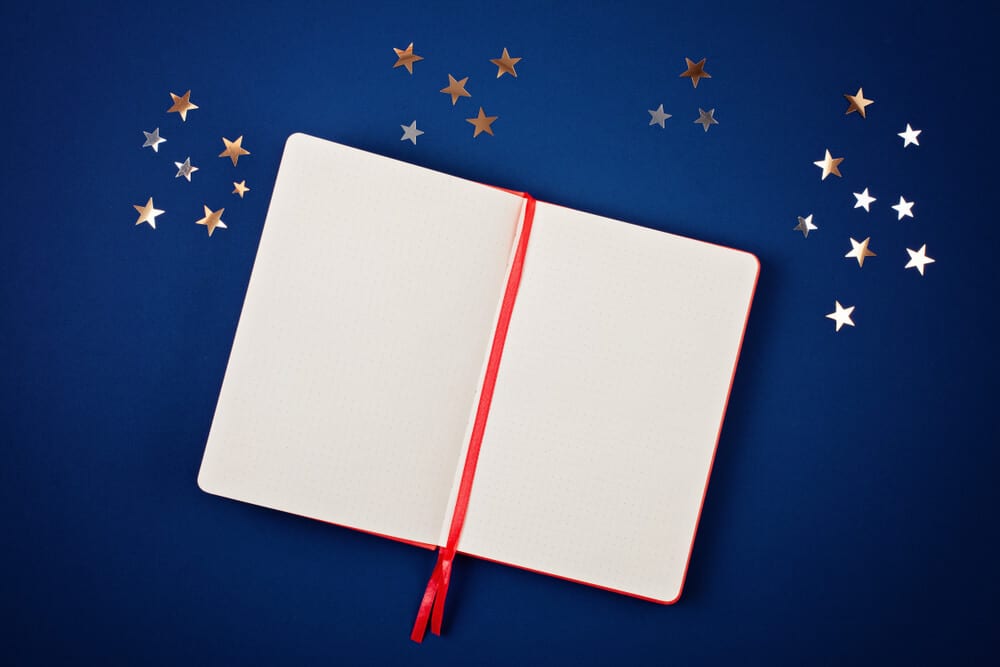
CBT-I involves personal reflection, hard work, persistence, and patience. Usually, the first step of any CBT-I plan is to keep a sleep journal for 1-2 weeks before doing anything else. Why? Well, a sleep diary will help someone note their sleeping habits, diet, exercise levels, thought patterns, emotions, and anything else that may relate to sleep quality. For the first week or two, this diary simply helps patients gain better insight into their own thoughts, feelings, and habits.
After tracking everything for 1-2 weeks, the groundwork begins. A patient and specialist can work together to analyze the sleep journal, evaluating anything that could be counterproductive to a good night’s rest. Then, they will work together to develop strategies the patient can use to change these counterproductive behaviors.
Now, just because the groundwork begins doesn’t mean a patient will stop writing in their diary. All the while a patient is working hard to change their habits, they will continue to keep a sleep journal. After all, these journals are great places to track both goals and progress.
Example Problem
For example, a journal might reveal that a university student does homework in bed and drinks caffeine well into the evening. Then, when the student doesn’t sleep well (which is often), she may begin to stress if she can sleep when she crawls into bed at night. In other words, this journal reveals that this student has poor hygiene habits:
- For starters, a bed should only be used for sleep and intimacy. Using it for anything else makes the brain associate it with other activities—aka, not sleeping, which means the body will take a longer time to feel drowsy sitting in a bed.
- Secondly, caffeine can affect the body hours after drinking it… up to 7 hours, in fact. That means it’s usually a good idea to cut off caffeine around noon.
- Thirdly, the student clearly stresses about sleep. While this stress is understandable, it actually makes her situation worse. Increased stress levels, after all, harm the ability to sleep and sleep well. Furthermore, when the student thinks of sleep, it’s often in a negative, stressful way, meaning the student associates sleep with anxiety. So, when the student lies down to sleep and worries if she can fall asleep. These racing thoughts stimulate the brain, making it harder to rest.
Example Solution
So, how would CBT-I help here?
CBT-I would force the student to address each of these issues in a progressive manner. So, the student would have to find a new place to complete homework as well as reduce caffeine intake and eliminate it after a certain time. Retraining her thoughts, naturally, will take more work.
It can be done, though.
One popular strategy for retraining sleep-related racing thoughts? Actually making time to worry that’s not bedtime. Ideally, this “worry time” will only be once a day, about 10-20 minutes long, and several hours before planned bedtime. This way, the student can take the time to address her concerns instead of repressing them. By dealing with them in a limited yet structured manner, she can prevent these thoughts from consuming her. Eventually, limiting worries to one time a day can help the brain associate bedtime with sleeping, not worrying.
How Long Does CBT I Take to Work?
Thoughts, emotions, and behaviors don’t develop overnight. That means it will take a bit to unlearn everything. Journaling itself will take a week or two. Patients will then have to actively work on their issues for several weeks after. Many treatment plans take several weeks, usually at least 4, but often 6 to 8. All in all, patients should expect to wait at least 5-6 weeks before noticing improvements.
How Do You Do CBT for Insomnia?
There are several methods for employing CBT-I, including in-person therapy with a specialist and digital therapy via websites and apps. There are also several books on the subject that may help.
Specialists

One tried-and-true method is speaking to a doctor. Options include speaking to primary care physicians and/or sleep specialists. To see AASM-accredited sleep centers, you can click here. For those on a limited budget, federally funded health centers might be the way to go. To discover such centers near you, you can click here.
Digital Therapy

Often used in conjunction with a healthcare provider, CBT-oriented apps may also help. One such app is CBT-i Coach, developed by the U.S. Department of Veteran Affairs. It is available for free here on Google Play and here on the Apple App Store.
Books

The 4-Week Insomnia Workbook by Sara Dittoe Barrett, PhD, may be a good place to start for book lovers. For starters, it includes all the necessary worksheets for keeping a detailed sleep journal. Even better, it helps readers develop a realistic 4-week plan (after journaling for 1 week prior), with new challenges introduced each week.
For those looking for a detailed yet easy-to-follow self-help book, this option is tough to beat. It’s available in paperback here on Amazon; Kindle Unlimited subscribers can download this book for free. Those who prefer audio should enjoy the fact that this title is available through Audible as well.
Final Thoughts

Everyone’s treatment plans will differ when it comes to battling insomnia. However, research shows that cognitive behavioral therapy for insomnia is currently one of, if not the, most effective strategies for dealing with this condition. While results aren’t immediate and it takes active work, the long-term benefits of CBT-I can far outweigh these “obstacles.”
Terms
- Acute Insomnia: Short-term insomnia.
- Chronic Insomnia: Long-term insomnia.
- Cognitive Behavioral Therapy (CBT): Talk therapy that reflection on thoughts, emotions, and behaviors to develop practical coping strategies.
- Cognitive Behavioral Therapy for Insomnia (CBT-I or CBT-i): CBT focused specifically on helping people achieve higher quality rest.
- Insomnia: A condition where someone can have issues falling and/or staying asleep.
- Primary Insomnia: Insomnia not caused by another medical condition.
- Secondary Insomnia: Insomnia caused by another condition.
- Sleep Hygiene: Another term for sleep-related habits.
- Sleep Onset Latency / Sleep Latency: How long it takes someone to fully fall asleep.
- Spielman Model: A widely accepted model for explaining chronic insomnia; predisposing factors(s), precipitating trigger(s), and perpetuating habit(s) are the three pillars of this model.
References
[9]Ağargün, M.Y., Kara, H., & Solmaz, M. (1997). Sleep disturbances and suicidal behavior in patients with major depression. Journal of clinical psychiatry, 58(6): 249-51. DOI: 10.4088/jcp.v58n0602
[4,13]Anderson K. N. (2018). Insomnia and cognitive behavioural therapy-how to assess your patient and why it should be a standard part of care. Journal of thoracic disease, 10(Suppl 1), S94–S102. doi:10.21037/jtd.2018.01.35
[2,7]Centers for Disease Control and Prevention. (2016). 1 in 3 adults don’t get enough sleep [Press release]. Retrieved from https://www.cdc.gov/media/releases/2016/p0215-enough-sleep.html
[12]Friedrich, A., Claßen, M., & Schlarb, A. A. (2018). Sleep better, feel better? Effects of a CBT-I and HT-I sleep training on mental health, quality of life and stress coping in university students: a randomized pilot controlled trial. BMC psychiatry, 18(1), 268. doi:10.1186/s12888-018-1860-2
[8]Genetic and rare diseases information center. (n.d.). Fatal familial insomnia. Retrieved from https://rarediseases.info.nih.gov/diseases/6429/fatal-familial-insomnia
[11]Institute for Quality and Efficiency in Health Care. (2006). Informedhealth.org. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK65083/
[10]Murphy, M. J., & Peterson, M. J. (2015). Sleep Disturbances in Depression. Sleep medicine clinics, 10(1), 17–23. doi:10.1016/j.jsmc.2014.11.009
[1,3,6]National Library of Medicine. (2016). Insomnia. Retrieved from https://medlineplus.gov/insomnia.html
[15]Sateia, M.J., Buysse, D.J., Krystal, A.D., Neubauer, D.N., & Heald, J.L. (2017). Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine clinical practice guideline. Journal of clinical sleep medicine, 13(2):307–349. Retrieved from http://dx.doi.org/10.5664/jcsm.6470
[5]Spielman, A.J., Caruso, L.S., & Glovinksy, P.B. (1987). A behavioral perspective on insomnia treatment. The psychiatric clinics in North America, 10(4): 541-53. PMID: 3332317
[14]Wagner, K. (2009). Cognitive behavior therapy is an effective treatment for chronic insomnia. American academy of sleep medicine. Retrieved from https://aasm.org/cognitive-behavioral-therapy-is-an-effective-treatment-for-chronic-insomnia/
Disclaimers
This article is not meant to substitute professional advice.